Laser Photocoagulation
Laser photocoagulation is done to reduce the risk of vision loss caused by diabetic retinopathy. It is most often used to stabilize vision and prevent future vision loss rather than to improve vision loss that has already occurred.
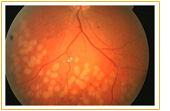
There are two approaches to treat diabetic retinopathy with laser photocoagulation. One is focal and the other is scatter (pan-retinal) type. Focal treatment is used to seal specific leaking blood vessels in a small area of the retina, usually near the macula. Scatter treatment is used to slow the growth of new abnormal blood vessels that have developed over a wide area of the retina. The ophthalmologist may make hundreds of laser burns on the retina to stop the blood vessels from growing. The person may need two or more treatment sessions.
Laser photocoagulation is usually performed as an outpatient procedure. It is not painful. The injection of anesthetic may be uncomfortable, and you may feel a slight stinging sensation or see brief flashes of light when the laser is applied to your eye.
Laser treatment is usually more beneficial if it is carried out early and the diabetes is well controlled.
Laser photocoagulation may be used to treat and prevent further progression of macular edema, which may occur in nonproliferative retinopathy. Focal photocoagulation is usually used in these cases.
Last Updated: October 23, 2024














