Age Related Macular Degeneration
What is age-related macular degeneration?
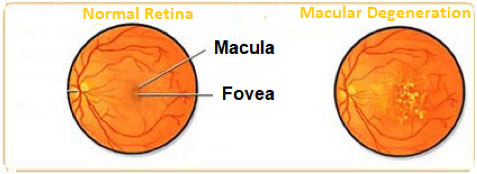
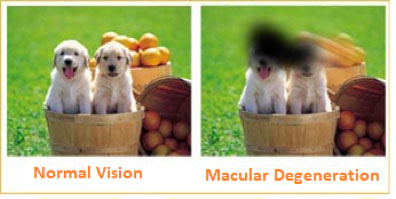
Age-related macular degeneration (AMD) is a common condition affecting people age 50 years and older. This condition is associated with the loss of retinal photoreceptor cells in the center of the retina where vision is the sharpest (the macula). Macula provides the sharp vision for reading, driving and seeing fine detail. But as a rule, age-related macular degeneration does not typically lead to complete blindness.
What increases risk for age-related macular degeneration?
The greatest risk factor for development of age-related macular degeneration is age. People who are older than 50 should get regular eye exams. Having a family member with age-related macular degeneration, smoking, high blood pressure, lighter eye color and obesity are among the risk factors developing age-related macular degeneration. Some researchers believe that over-exposure to sunlight also may be a contributing factor in development of macular degeneration. Women appear to be at greater risk than men. Lifestyle can play a role in reducing the risk of developing age-related macular degeneration. Eating a healthy diet high in green leafy vegetables and fish is assumed to protect against age-related macular degeneration.
What are the symptoms of age-related macular degeneration?
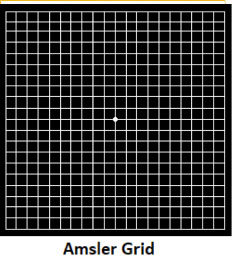
When the person starts experiencing visual problems from age-related macular degeneration, symptoms can include: blurred vision, blurry areas on a printed page, difficulty reading in low light levels or straight lines appearing wavy or distorted. Age-related macular degeneration reduces vision in the central part of the retina, it does not affect the peripheral vision.The early stages of macular degeneration can be detected by a simple test using a chart called the Amsler grid. Waviness, distortion, or missing lines on the grid may be noticed before a change in visual acuity.
What are the types of age-related macular degeneration?
Clinically, there are two types of age related macular degeneration‘’dry’’ (non-neovascular) and ‘’wet’’ (neovascular) form. The dry age related macular degeneration is the most common form. It accounts for about 90% of age related macular degeneration cases and is caused by aging of the macula. Vision loss is usually gradual. Deposits under the retina called "drusen" are a common feature of dry macular degeneration. Drusen alone usually do not cause vision loss, but when they increase in size or number some people will advance to central vision loss due to geographic atrophy which is the end stage of dry form.
The "wet" form of age related macular degeneration is a late stage of the condition and accounts for about 10% of all cases. Unfortunately, it accounts for the majority of central vision loss due to age related macular degeneration. Vision loss may be rapid and severe. The wet type implies leakage and bleeding in the macula due to abnormal blood vessels known as choroidal neovascularization. Left untreated, these abnormal blood vessels will grow and eventually cause scarring with permanent vision loss.
How is age-related macular degeneration diagnosed?
To diagnose age-related macular degeneration effectively the following procedures are commonly performed: distance and near vision acuity tests, a dilated fundus examination, optical coherence tomography to obtain a clearer picture of the macula and its supporting layers, optical coherence tomography angiography and dye assisted angiography to find abnormal blood vessels under the retina.
How is age-related macular degeneration treated?
Currently, the only treatment for dry age-related macular degeneration is dietary vitamin and other supplements. The AREDS (Age Related Eye Disease Study) has found that a certain combination of vitamins (vitamins C and E, lutein, zeaxanthin, and zinc) can slow the progression of dry age-related macular degeneration in people with a moderate level of disease. However, these vitamins do not cure age-related macular degeneration. The treatment of wet age-related macular degeneration has changed rapidly over the past few years.Treatment of this condition with intravitreal anti-VEGF (Vascular Endothelial Growth Factor) monotherapy is currently the standard of care. These drugs block the development of new blood vessels and limit the leakage from these vessels. They are delivered through an injection into the eye and several injections over time are usually needed. In certain types of neovascularization photodynamic therapy (PDT) can be used. Photodynamic therapy utilises a laser beam with a light-sensitive dye to destroy unhealthy new blood vessels in or under the retina.
Last Updated: October 23, 2024



























