Diabetic Retinopathy
What is Diabetic Retinopathy?
Diabetic retinopathy is an eye problem caused by diabetes mellitus. It affects the retina, which is light-sensitive tissue at the back of the eye. Retinopathy occurs when diabetes damages the tiny blood vessels in the retina. This damage can lead to problems with your vision, including blindness. Diabetic retinopathy is the most common cause of blindness due to diabetes mellitus.
Do all diabetic patients have retinopathy?
It is an ocular manifestation of systemic disease which affects up to 80% of all patients who have had diabetes for 10 years or more.
As long as a patient has diabetes, there is a chance for retinopathy. Early diagnosis and treatment can prevent vision loss. Careful control of your blood sugar level, blood pressure, and cholesterol will help delay and possibly prevent vision loss.
At first, diabetic retinopathy may cause no symptoms or only mild vision problems. The abnormal growth of new blood vessels in the retina can lead to serious vision problems such as vitreous hemorrhage, retinal detachment or glaucoma. Eventually, however, diabetic retinopathy can result in blindness.
Diabetic retinopathy is usually classified as early or advanced.
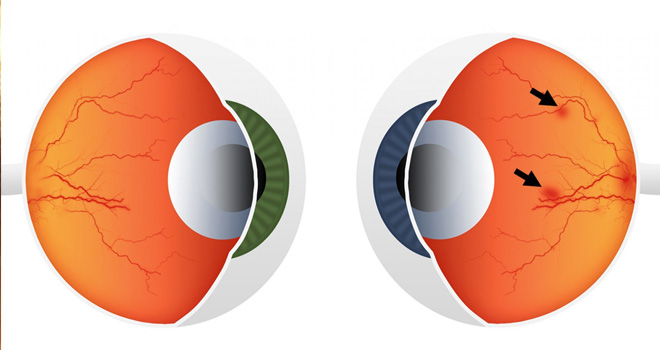
Early diabetic retinopathy. Nonproliferative diabetic retinopathy (NPDR) is the most common type of diabetic retinopathy. It can be described as mild, moderate or severe. When you have NPDR, the walls of the blood vessels in your retina weaken. Tiny bulges protrude from the vessel walls, sometimes leaking or oozing fluid and blood into the retina. These bulges are called microaneurysms. As the condition progresses, the smaller vessels may close entirely and the larger retinal veins may begin to dilate and become irregular in diameter. Nerve fibers in the retina may begin to swell. Sometimes the central part of the retina (macula) begins to swell, too. This is known as macular edema.
Advanced diabetic retinopathy. Proliferative diabetic retinopathy (PDR) is the most severe type of diabetic retinopathy. When you have PDR, abnormal blood vessels grow in the retina. Sometimes the new blood vessels grow or leak into the clear, jelly-like substance that fills the center of your eye (vitreous). Eventually, scar tissue stimulated by the growth of new blood vessels may cause the retina to detach from the back of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure may build up in the eyeball. This can damage the nerve that carries images from your eye to your brain (optic nerve). Diabetic retinopathy can happen to anyone who has diabetes. The risk of diabetic retinopathy is highest if the patient has
Has poor control of your blood sugar level
Has high blood pressure
Has high cholesterol
Smokes
Often there are no symptoms in the early stages of diabetic retinopathy. Diabetic retinopathy begins before a patient has any symptoms. As the problem gets worse blurred vision and floaters are seen.
Diabetic retinopathy is best diagnosed with a dilated eye exam. During the exam, doctor looks for:
Abnormal blood vessels
Swelling, blood or fatty deposits in the retina
Damage to the nerve tissue
Growth of new blood vessels and scar tissue
Bleeding in the center of the eye
Retinal detachment
How is diabetic retinopathy diagnosed?
As part of the eye exam, your doctor may do a retinal photography test called fluorescein angiography. First, your doctor will dilate your pupils and take pictures of the inside of your eyes. Then a special dye will be injected into a vein in your arm. More pictures will be taken as the dye circulates through your eyes. Your doctor can use the images to pinpoint blood vessels that are closed, broken down or leaking fluid.
Your doctor also may request an optical coherence tomography (OCT) exam. This imaging test provides cross-sectional images of the retina that show the thickness of the retina and whether fluid has leaked into retinal tissue. Later, OCT exams can be used to monitor treatment effectiveness.
What is the treatment of diabetic retinopathy?
Prevention is the best treatment for diabetic retinopathy. Strict control of blood sugar will significantly reduce the long-term risk of vision loss.
Treatment for diabetic retinopathy depends on the type of diabetic retinopathy you have, its severity and how well it may respond to specific treatments.
The first option for diabetic macular edema treatment is intravitreal injection of anti-VEGF or steroids.
If abnormal blood vessels have grown on the retina (proliferative diabetic retinopathy), laser surgery can be effective in shrinking those vessels and preventing them from growing in the future. Multiple laser treatments over time are sometimes necessary. Laser surgery does not cure diabetic retinopathy and does not always prevent further loss of vision.
If there is advanced damage to the eye because of retinopathy, a microsurgery called vitrectomy may help.
Last Updated: October 23, 2024



























